As of May 2, Canadian long-term care residents accounted for 63 per cent of all deaths from COVID-19. According to the International Long-Term Care Policy Network (ILTCPN), Canada has the highest share of deaths in long-term care homes of 13 countries.
The Public Health Agency of Canada puts that number higher. The agency says 82 per cent of coronavirus-related deaths in Canada have taken place in long-term care homes.
Northwood is the largest long-term care home in the Atlantic region. It is a not-for-profit facility, run by a community board and located in central Halifax. Forty-one residents have died from COVID-19 since the pandemic began nearly two months ago. That accounts for 87 per cent of the coronavirus deaths in Nova Scotia. All told, there have been 47 deaths in the province. As of May 8, 229 Northwood residents and 95 staff tested positive for COVID-19. Some residents who have recovered have been moved to a nearby hotel, as the designated recovery rooms at Northwood are full.
How can Northwood, the pre-eminent “public” care facility in Nova Scotia, one that was only last year accredited “with exemplary standing,” be in such a desperate situation now?
Several problems have converged — most were predictable, some were not. But these issues shine a light on some of the reasons why COVID-19 is raging through long-term care facilities across Canada.
Design of nursing homes: Built on a mini-hospital model
First, like many long-term care homes across the country, many of the 485 residents of Northwood are living two and three to a room, and they share a bathroom. It resembles a hospital in several ways.
Built in 1962, Northwood is a large institution, with dozens of rooms down each side of long windowless corridors in a 10-storey building. It is crowded; there is little privacy. Residents spend time in the hallways and the common spaces. The close contact between residents, and between residents and staff, could be a breeding ground for any influenza, or communicable disease. Nursing home designers and architects have to answer for building institutions on this model.
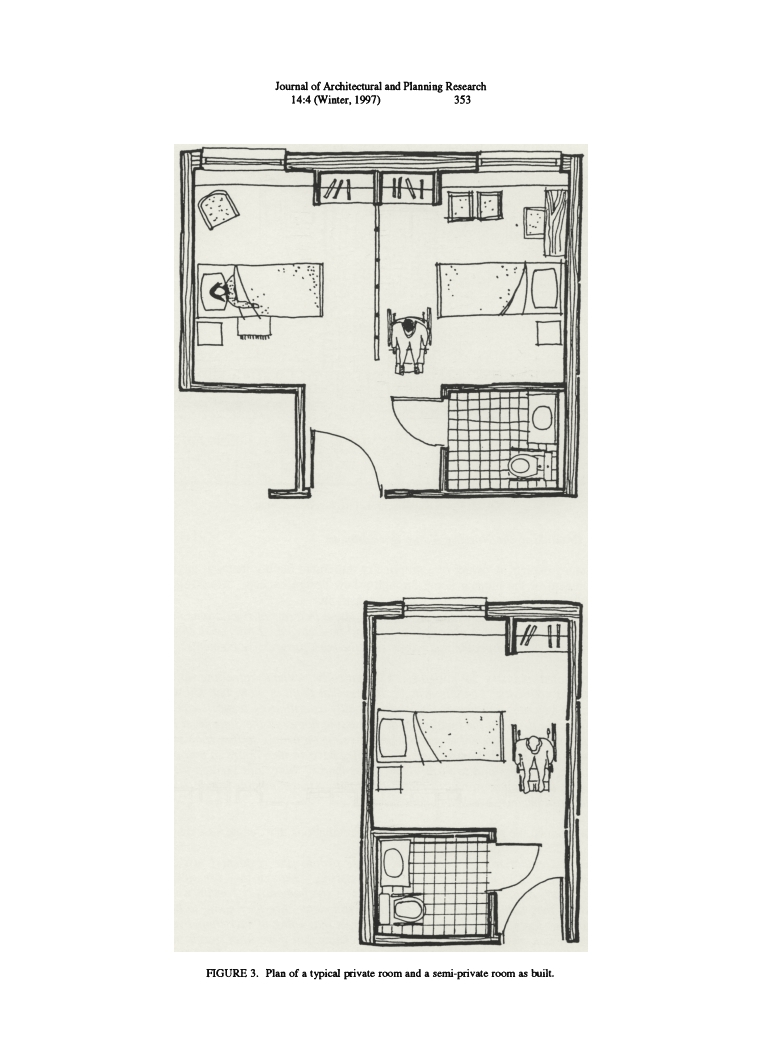
A drawing of a private and semi-private long-term care room from Schwarz's article "Nursing Home Design"
According to one U.S.-based architecture professor, Benyamin Schwarz, nursing home design seems to “clash with efforts to satisfy the non-medical needs of the frail elderly.” Schwarz writes that nursing homes must cater to competing interests, which include those of the residents, the medical teams, the government that controls their financial strings, the institutions’ economic exigencies and the social needs of the senior community.
According to Schwarz, “… the public health services experts who drew up the requirements (for nursing homes) were heavily affected by their hospital orientation, which is why to this day most nursing homes look so much like mini-hospitals.”
Nursing home design from 50 or 60 years ago often had residents share a room, which allowed the home to house more seniors, more cheaply. This was an incentive for the privately owned nursing homes. But two to four to a room can present serious risks to residents’ health. For for-profit long-term care homes, economizing is attractive because when they double-bunk, their profits ratio go up. While profit is not an incentive for Northwood in Halifax, accommodating two or three to a room does increase capacity, without the cost of building a new or expanded structure.
Aside from the obvious health risks, nursing homes’ box-like and crowded settings are themselves a problem. As Schwarz points out, “If the depressing and frightening setting of the American nursing home reflects our collective moral heart — it is fairly grim.”
Above are drawings of a traditional double room and a single room for a conventional nursing home. Here’s how most nursing homes are designed: the long hallways, with little natural light, mean residents park themselves in their wheelchairs in the hallways to enable easier social contact.

Schwarz finishes his article this way: “Society should be able to create a better architectural model for frail elderly which asserts their rights and freedoms for a fulfilling old age. This is not a utopian goal.”
Cuts to long-term care budgets
Two successive Stephen McNeil governments have cut the budgets of most of the province’s 132 nursing homes and residential care facilities. From 2015 to 2017, Premier McNeil’s Liberal government reduced grants to long-term care by $8.1 million.
Northwood’s president and CEO, Janet Simm, said the 2016 cuts amounted to $360,000 for her institution; in 2017, the cut was nearly $600,000.
While Northwood turned to group purchasing and other measures to economize, the biggest challenge was food. In part, this was because more and more residents had special diets. On average, N.S. nursing homes spent $6 per resident per day for food. Some residents complained that a meal supplement drink (such as Boost) was offered at meal times in order to trim the food bills.
Cuts to food
Northwood’s Simm said, “With rising costs of food and the decreasing budget, it’s a real challenge to meet the growing demands. This is where people live and you want to make sure the food is high-quality because it is a big piece of quality of life.”
Unifor, the union that represents more than 400 workers at Northwood, agreed that the quality of care was affected by the funding cuts; staff hours were also reduced, so staff noticed they had less contact time with residents.
This photo of a plate of baked beans and potatoes was taken by Colin Sproul, April 29, 2017, a month before the provincial election.

This was the meal served to Sproul’s mother at a transitional care unit inside Middleton Soldiers Memorial Hospital in the Annapolis Valley, N.S., where his mother had been waiting for a long-term care bed. Sproul said, “This is a direct consequence of Stephen McNeil’s cuts in Annapolis County and the effect it’s having on people.” Sproul was the NDP candidate in Premier McNeil’s riding of Annapolis.
It was just before the May 2017 election that I ran into the premier himself, who was electioneering along the boardwalk on Halifax’s waterfront. I stopped him, introduced myself, and asked him if he would have cut a nursing home’s food budget if his mother had lived there. He became furious – so angry that his principal secretary at the time, former CTV news reporter Laurie Graham, had to pull him away, insisting they had to go.
Just before the May 2017 election, NDP leader Gary Burrill, in a bid to restore the $8.1 million McNeil’s government cut from long-term care, promised that, if elected, an NDP government would put $8.3 million back into long-term care.
In his 2017-18 budget, McNeil reinstated $3.2 million.
Then, in the 2019-20 budget, the government added a further $2.8 million. But to fully restore that initial $8.1 million and inflation, the government would have had to add $8,764,120. Instead, the McNeil government restored a total of $6,000,000 — a net loss of funding to long-term care of $2,764,120.
However, from 2013 to 2016, McNeil did put $55 million into homecare. The idea was to support seniors who wanted to stay in their own homes. In fact, at the time, increased funding for homecare was a trend in government budgets right across the country.
Though Anthony Taylor agreed homecare deserved to be bolstered, he did not think it should have been at the cost of long-term care. Taylor is the administrator of a 111-bed nursing home, Oakwood Terrace, in Dartmouth, N.S. In 2015, Oakwood suffered a budget cut of $82,000, and in 2016 another cut of $86,000. Said Taylor, “Those two years, back to back, this government has cut more money from this nursing home than any other government has done to this home in the 34 years we have existed.”
The crisis in staffing: before and during COVID-19
Finally, there is the urgent issue of staffing before and during the COVID-19 crisis. Provincial regulations call for one Licensed Practical Nurse (LPN) to care for up to 30 residents, and a Registered Nurse (RN) to be on the premises 24 hours a day. Both of these rules have been contravened many times in nursing homes across Nova Scotia, which frequently “run short” — meaning fewer care workers are on the job than needed.
In Nova Scotia, long-term care homes are workplaces that pay from $17 to $25 per hour (of course, the RNs earn more). Before you call that a good wage, think about this: Would you do the physically demanding and tedious work of an LPN, or a personal care worker (PCW), for that wage? Given full time hours, you could earn about $40,000 per year.
However, in Nova Scotia, with the budget cuts to long-term care, many care workers whose hours were cut in one home had work at part-time jobs at one or two other long-term care homes to earn enough to live. Until recently, there was no restriction on the number of care homes at which staff were allowed to work.
Nearly four weeks ago, in response to the pandemic, Ontario’s premier issued an emergency order that prohibits nursing home staff from working at more than one facility. This was done to help contain transmission of the virus by the staff who could carry it from one care home to another.
Premier McNeil declared no such rule in Nova Scotia. In fact, having staff work at two or three homes worked in the government’s favour, because there was little pressure to raise wages. Until the arrival of COVID-19, no one seemed to care that staff were going in and out of Northwood and other nursing homes, wearing the same clothes, and potentially becoming vectors for disease.
As of April 23, Nova Scotia was one of the last provinces to discourage staff from working at more than one long-term care facility.
Historically, employees in long-term care facilities earn less than what they would in an acute care hospital. On May 7, the McNeil government finally agreed to give a pay increase to front-line workers in nursing homes, backdated to March 13. Rather than offering a top-up on their hourly pay, the Nova Scotia government insists on paying the care workers a bonus of $2,000 for the estimated four month duration of the COVID-19 crisis.
As there is high demand for care workers, who are finally getting 35- to 40-hour work weeks, employees will receive the bonus, which works out $2.90 an hour. The sticking point is they have to have worked the whole four months, and won’t collect if they fall sick themselves.
Dangers in confined or crowded spaces
This brings us to the point about dangers facing groups of people in confined spaces. Nova Scotia closed all schools, from daycares to universities. Gyms, libraries, theatres and community centres also had to shut. But there was little to no attention paid to nursing homes and elder care residences.
However, many public health experts know how dangerous viruses can be to residents of nursing homes. According to an article in the journal Clinical Infectious Diseases: “The common occurrence and dire consequences of infections disease outbreaks in nursing homes often go unrecognized and unappreciated. Nevertheless, these facilities provide an ideal environment for acquisition and spread of infection: susceptible residents who share sources of air, food, water, and health care in a crowded institutional setting. Moreover, visitors, staff, and residents constantly come and go, bringing in pathogens from both the hospital and the community.”
While nursing homes could not be closed, arrangements could have been made. The arrangements we see at Northwood today, such as devoting a floor of the building to isolating those who test positive, or assigning a floor to those recovering, made around April 20th, could have been made sooner. And when did Northwood begin spatial distancing measures such as moving people from double to single rooms, or if that option was off the table, moving some healthier residents who required less care to hotel rooms?
Pandemic and prisons
Public Health warned us a pandemic was coming to all regions of Canada. By early March we all knew. Now, eight weeks later, as a result of mandatory social-distancing and isolation, we are seeing a slight fall in the community spread, but deaths in nursing home are still rising.

Prisoner rights activists, and lawyers representing prisoners, have warned us that prisons will become a killing ground for prisoners and jailers alike once COVID-19 begins to spread inside. The prison guards go home to their families after their shifts, and return to the jail every workday.
We didn’t heed the warnings in time to save thousands of elderly people in institutions across the country. Are we listening to the warnings about the risk to the prison populations? They will be the next COVID-19 frontier.



Comments